Title : Halving broken hips in hospital – The pivotal value of nursing leadership in New Zealand
Abstract:
Introduction: Sitting alongside my role of director of nursing patient safety and quality of a public hospital is my role as clinical lead to the Commission’s reducing harm from falls programme in New Zealand. I have a unique opportunity to influence the collective power of the senior nursing workforce.
The Commission oversees the national quality improvement programme to reduce harm from people falling in care settings – hospital, aged residential care – and those receiving care at home. Nurses are well placed to improve patient outcomes as they are at the bedside 24 hours and plan for community care.
Falls are recognised internationally as a nurse indicator of care, yet evidence has not identified sustainable strategies to reduce patients falling and fracturing hips. Measuring and understanding falls enable nurses to “make more informed decisions about care-based criteria and ultimately such measures provide us with an opportunity to really make the quality of nursing care count” (Griffiths P, The Kings Fund, London, England, 2008).
Voluntary serious adverse event reporting revealed falls were the most-reported event in New Zealand hospitals.
• In 2014, 137.6 per 1000 New Zealanders aged 50 or over had an insurance claim accepted for a fall-related injury (up 20% since 2011).
• More than 3640 people over 50 (2.4 per 1000) presented with a hip fracture in 2014, directly costing NZ$171m.
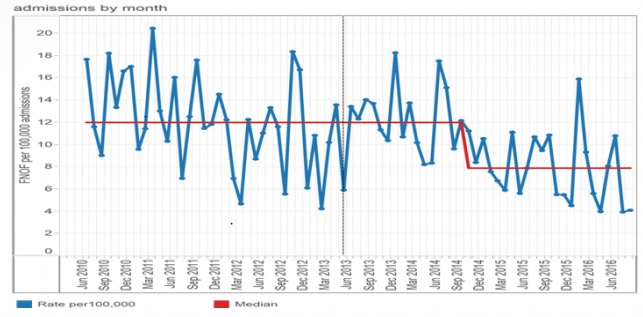
• In 2012, two patients fell and broke their hips in hospitals each week with a conservative cost per incident of NZ$47,000. In 2015-16 this rate reduced to four every three weeks.
A fall is a complex interaction between a person’s risk factors and environment. No single solution reduces harm but an essential first step is to identify the individual’s risks of falling and develop a tailored prevention plan informed by that individual’s risk factors.
This first step evolved into the development of the national falls quality and safety process markers which measure risk assessments and care planning. A suite of evidence-based resources were developed to build capability and support nurses to make the right care choices, put evidence into practice and use the tools developed. A Falls Atlas of Healthcare Variation was also developed to show national and local variation to inform quality improvement more broadly than the hospital setting. The ethos of ‘aggregation of marginal gains’ helped avoid overwhelming organisation capacity while nurses working in multidisciplinary teams avoided tribalism and supported an adaptive organic model of improvement.
Results:
• Patients aged 75 and older provided with a falls risk assessment increased from 76% to 92% in December 2015; the percentage provided with an individualised care plan increased from 80% to 92%.
• A 41% reduction in in-hospital falls associated with fractured neck of femur to December 2015, and savings to public hospitals of US$1.9 million (NZ$2.8 million).
Conclusion: A nurse-led comprehensive, integrated quality improvement programme approach resulted in a statistically significant reduction in in-patient falls with a fractured neck of femur in New Zealand public hospitals.
Audience Take Away
• Developing and holding on to a vision to reduce patient harm supported by a focus on measurement for improvement.
• Pragmatically translating evidence into practice at the bedside.
• Increase understanding of the power of senior nurses working collaboratively with other members the health sector and each other to lead reducing harm from falls.
• Reinforcing nurses’ ability to influence patient outcomes as evidenced by reduced fractured hips in New Zealand hospitals.
• Access to New Zealand’s evidence-based tools including a computerized nursing risk assessment



